
Opus Spark November 2022
Veterans with PTSD During the Holidays
Message from the CEO
This month we recognize and honor our Veterans who have served our country and have suffered mental health outcomes. For those who have veterans as patients, family members, or friends, it is important to understand them better and offer the support they need, especially during the holidays.
For those who suffer from Post-Traumatic Stress Disorder (PTSD), the holiday season can be an especially difficult time of year. People with PTSD can struggle with memories of traumatic events that may have occurred in the past, while they may also feel anxious or isolated from friends and family members.
Therefore, it is important for us to take extra steps to ensure that veterans with PTSD are supported during this time of year. Here are a few suggestions on how we can support those with PTSD during the holidays:
- Offer emotional and practical support. Take time to listen to their stories, share comforting words, or provide assistance with daily tasks like grocery shopping or running errands.
- Create a safe space for them. If possible, create a comfortable place in your home where they can talk about their experiences without feeling overwhelmed or judged.
- Show gratitude during Thanksgiving. Expressing appreciation for our veterans and those who have served is one of the best ways to show our respect and admiration for their courage and dedication.
- It can also help remind them that they are not alone in their struggles and serve as an important reminder of all the good they have done for our country. Consider sending a card or letter expressing your gratitude.
- Reach out to organizations that support veterans with PTSD. There are many organizations dedicated to helping veterans cope with PTSD. Contact a local organization or reach out online to find more information about how you can lend your support.
- Provide educational resources on PTSD. Knowing more about the disorder can help you better support veterans suffering from PTSD. Look for books, articles, and websites that provide helpful information about PTSD, so you can be prepared to offer your assistance in the best way possible.
Let’s remember Veterans who suffer from PTSD by being mindful of those struggling and ensuring they have all the support they need to get through the holidays safely and happily.
Thank you for taking the time to learn more about how we can support veterans with PTSD during this special time of year. By coming together as a community, we can make sure they are given all the care and respect they deserve.
We wish you and yours a very Happy Thanksgiving!
Trey Wilson
Chief Executive Officer
Opus Behavioral Health
Clinician of The Month

Jamie Brown is the Childcare Coordinator, Counselor, and Educator at Options for Recovery and is celebrated for her impact on her patients and team. Her team acknowledges her as being one of the most humble, gracious yet dedicated clinicians I have ever met. She is easy to teach and an amazing team player. She is highly skilled and talented.
Back in 2011, while pursuing her bachelor’s in human services from California State University, she got the wonderful opportunity to intern at Options for Recovery for a semester. After acquiring her degree, she got hired towards having a successful career working with adults with intellectual disabilities. She returned to the agency in 2018 as Options Childcare Coordinator and in 2022, she was given the additional role of Counselor/Educator. While working with women in all areas of their lives, her focus was on increasing their parenting skills by addressing their parental shame/guilt, increasing healthy coping skills, and helping them change unhealthy patterns learned throughout their lives. She feels the most important part of her job is to provide an unbiased space for the women she works with so they can discover who they are and cultivate parenting skills to help them become the parents they wish to be.
Jamie is dedicated, empathetic, and able to build rapport with clients and professionals. She teaches parenting classes and addiction classes. Her ability to connect with clients individually and in a group is dynamic. Clients share their strengths in reconnecting with their children after using Jamie's techniques and suggestions. She understands the impact that addiction can have on relationships and parenting. Her calm approach and direct demeanor make clients feel safe and supported. She is professional and knowledgeable in several areas and does not fret about sharing her knowledge with peers and clients.
Jamie has impacted many clients within the last 7 years of her time at the agency. Jamie assisted a client with limited parenting skills and major health challenges. Work through several medical treatments, and parent simultaneously by using her suggested strategies. This client is stable and sober today, and her relationship with her son is remarkable. Jamie was able to help her through many difficult procedures and inspired her to continue with her recovery goals while being a new mom.
Digging Deeper in Understanding PTSD:
.png?width=762&height=487&name=veterans%20newsletter%20(PTSD%20sec).png)
What is PTSD:
Post-traumatic stress disorder is a mental health condition that's triggered by a terrifying event — either experiencing it or witnessing it. Symptoms may include flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event.
Most people who go through traumatic events may have temporary difficulty adjusting and coping, but with time and good self-care, they usually get better. If the symptoms get worse, last for months or even years, and interfere with your day-to-day functioning, you may have PTSD.
Getting effective treatment after PTSD symptoms develop can be critical to reducing symptoms and improving function.
What are the symptoms:
Post-traumatic stress disorder symptoms may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions. Symptoms can vary over time or vary from person to person.
Intrusive memories
Symptoms of intrusive memories may include:
- Recurrent, unwanted distressing memories of the traumatic event
- Reliving the traumatic event as if it were happening again (flashbacks)
- Upsetting dreams or nightmares about the traumatic event
- Severe emotional distress or physical reactions to something that reminds you of the traumatic event
Avoidance
Symptoms of avoidance may include:
- Trying to avoid thinking or talking about the traumatic event
- Avoiding places, activities or people that remind you of the traumatic event
Negative changes in thinking and mood
Symptoms of negative changes in thinking and mood may include:
- Negative thoughts about yourself, other people or the world
- Hopelessness about the future
- Memory problems, including not remembering important aspects of the traumatic event
- Difficulty maintaining close relationships
- Feeling detached from family and friends
- Lack of interest in activities you once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally numb
Changes in physical and emotional reactions
Symptoms of changes in physical and emotional reactions (also called arousal symptoms) may include:
- Being easily startled or frightened
- Always being on guard for danger
- Self-destructive behavior, such as drinking too much or driving too fast
- Trouble sleeping
- Trouble concentrating
- Irritability, angry outbursts, or aggressive behavior
- Overwhelming guilt or shame
For children 6 years old and younger, signs and symptoms may also include:
- Re-enacting the traumatic event or aspects of the traumatic event through play
- Frightening dreams that may or may not include aspects of the traumatic event
Intensity of symptoms
PTSD symptoms can vary in intensity over time. You may have more PTSD symptoms when you're stressed in general, or when you come across reminders of what you went through. For example, you may hear a car backfire and relive combat experiences. Or you may see a report on the news about a sexual assault and feel overcome by memories of your own assault.
When to see clinical treatment:
If you have disturbing thoughts and feelings about a traumatic event for more than a month, if they're severe, or if you feel you're having trouble getting your life back under control, talk to your doctor or a mental health professional. Getting treatment as soon as possible can help prevent PTSD symptoms from getting worse.
If you have suicidal thoughts
If you or someone you know has suicidal thoughts, get help right away through one or more of these resources:
- Reach out to a close friend or loved one.
- Contact a minister, a spiritual leader, or someone in your faith community.
- Call a suicide hotline in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to reach a trained counselor. Use that same number and press 1 to reach the Veterans Crisis Line.
- Make an appointment with your doctor or mental health professional.
What are the causes:
You can develop post-traumatic stress disorder when you go through, see or learn about an event involving actual or threatened death, serious injury, or sexual violation.
Clinicians aren't sure why some people get PTSD. As with most mental health problems, PTSD is probably caused by a complex mix of:
- Stressful experiences, including the amount and severity of trauma you've gone through in your life
- Inherited mental health risks, such as a family history of anxiety and depression
- Inherited features of your personality — often called your temperament
- The way your brain regulates the chemicals and hormones your body releases in response to stress
What are the risk factors:
People of all ages can have post-traumatic stress disorder. However, some factors may make you more likely to develop PTSD after a traumatic event, such as:
- Experiencing intense or long-lasting trauma
- Having experienced other trauma earlier in life, such as childhood abuse
- Having a job that increases your risk of being exposed to traumatic events, such as military personnel and first responders
- Having other mental health problems, such as anxiety or depression
- Having problems with substance misuse, such as excess drinking or drug use
- Lacking a good support system of family and friends
- Having blood relatives with mental health problems, including anxiety or depression
Kinds of traumatic events
The most common events leading to the development of PTSD include:
- Combat exposure
- Childhood physical abuse
- Sexual violence
- Physical assault
- Being threatened with a weapon
- An accident
Many other traumatic events also can lead to PTSD, such as fire, natural disaster, mugging, robbery, plane crash, torture, kidnapping, life-threatening medical diagnosis, terrorist attack, and other extreme or life-threatening events.
What are the complications: post-traumatic stress disorder can disrupt your whole life ― your job, relationships, health, and enjoyment of everyday activities.
Having PTSD may also increase your risk of other mental health problems, such as:
- Depression and anxiety
- Issues with drug or alcohol use
- Eating disorders
- Suicidal thoughts and actions
What can be done to prevent PTSD:
After surviving a traumatic event, many people have PTSD-like symptoms at first, such as being unable to stop thinking about what's happened. Fear, anxiety, anger, depression, and guilt are common reactions to trauma. However, many people exposed to trauma do not develop long-term post-traumatic stress disorder.
Getting timely help and support may prevent normal stress reactions from getting worse and developing into PTSD. This may mean turning to family and friends who will listen and offer comfort. It may mean seeking out a mental health professional for a brief course of therapy. Some people may also find it helpful to turn to their faith community. Support from others also may help prevent you from turning to unhealthy coping methods, such as misuse of alcohol or drugs. (Cited from Mayo Clinic, 2022)
Opus EHR has Standard and Customizable PTSD Screenings to Measure Outcomes
The PTSD screening tool enables patients to receive and complete assessments remotely via text/mobile or email. The outcome measurement gives clinicians a visual of their most recent assessments while creating new documentation. The Beck Depression Inventory assessment is widely used, and Opus can accommodate other assessments pertaining to each facility's needs. The PTSD screening tool allows practices to have:
- Full collection of industry-standard assessments to choose those that best fit your practice
- Create and integrate your own scoring assessments to accurately measure outcomes
- Visualize and report on client scores using graphs and see what’s trending throughout the treatment
- Create and administer custom surveys and assessments (e.g. patient satisfaction survey)
- Automate the administration of scales to a client portal to ensure score acquisition
- Report on client scores
To learn more on how to use this tool with Opus EHR, schedule a consultation with our experts: https://bit.ly/opusehr
Holiday Tips on practicing a Gratitude State of Mind during:
- Appreciate the relationships you have
- Bringing more positivity to each interaction daily
- Having a gratitude journal
- Saying Thank you to those that are closest, so they know you appreciate them
- Create a workout routine
- Volunteer in your community
- Get better sleep (average 7-8 hours)
- Eating fruits and vegetables daily
Resources for Veterans suffering PTSD
Many resources are available online and in person for veterans with PTSD during the holiday season. Some of these resources include support groups, therapy, and medication. If you are feeling overwhelmed or discouraged during the holiday season, please don't hesitate to seek help from a professional. You are not alone in dealing with PTSD, and there are many people who want to help you manage your symptoms. Some resources include:
https://drugrehabus.org/rehabs/treatment/veterans/united-states/
https://www.findhelp.org/
https://www.va.gov/directory/guide/sud.asp
https://www.va.gov/directory/guide/state_SUD.cfm?STATE=FL https://www.mentalhealth.va.gov/substance-use/index.asp
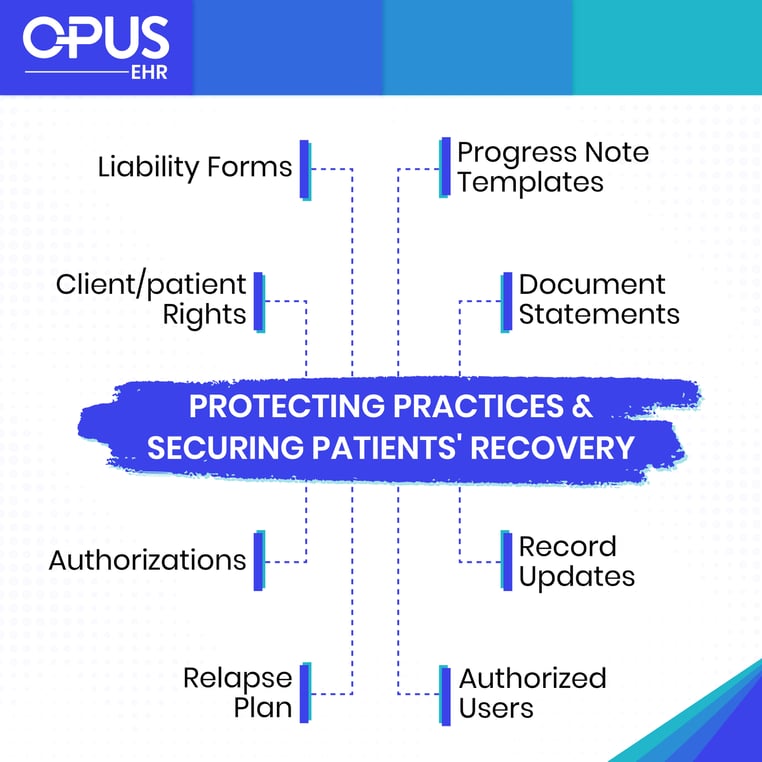
Feature of the Month: Forms and Documents to Reduce AMA/ACA
During the holidays, patients and clients can get discouraged and leave against medical advice or against clinical advice. It is important to have the most effective tools to help make processes efficient to support practice operations, especially during the holidays. To protect you and other health care providers caring for the patient and your facility if problems were to arise from an unapproved discharge, you should have the patient sign an AMA form. These forms should clearly document that the patient knows he's leaving AMA, that he's been advised of and understands the risks of leaving, and that he knows he can come back. The AMA form should include an explanation of the risks, and names of those involved. The progress notes, document statements, and actions reflect the patient's mental state when he left your facility. This helps protect you and other health care providers caring for the patient and the facility against a charge of negligence if the patient later claims that he was mentally incompetent at the time of discharge and was improperly supervised while in that state.
Also, progress note templates, and document statements that reflect the patient's mental state before, during, and at the time he/she left the facility. This helps protect practices and health care providers caring for the patient and the facility against a charge of negligence if the patient later claims that he was mentally incompetent at the time of discharge and was improperly supervised while in that state.
Opus EHR has template forms, documents, and waivers in the library for practices to conveniently have them on hand when needed, including:
- Consent to Treatment (liability form)
- Authorization for the release of information
- Assignment of benefits/ Release of medical information
- Confidentiality of mental Health client records
- Client rights
- Relapse Plan
- Grievance and Appeals Process
- Uses and Disclosure of Health Information
- Refund policy
- Confidentiality Agreement
- Client AMA Self-Blocking Assessment
- Progress notes templates
Our team is constantly adding new tools and features and practice needs as we get feedback from our valued clients. If you are interested in upgrading your operations by giving Opus EHR a try, we offer a demo https://bit.ly/opusehrdemo and a 21-day free trial (https://bit.ly/opustrial).
